Strong anesthesiology care is an integral part of any well-functioning procedural services department, and many anesthesia providers have taken on expanded roles in pre-surgical patient optimization, non-operating room areas (NORA), and critical care settings to help their hospital partners weather the storm.3
While many of these trends were long on the horizon, rapid changes to daily clinical routines have made anesthesia operations increasingly inscrutable to key stakeholders like nursing leadership, surgeons, and hospital administration. Many anesthesia groups struggle to predict what their footprint will be on any given day, and failure to proactively communicate coverage changes can inculcate distrust and skepticism about anesthesia providers’ commitment to the needs of the organization. Often finding themselves in contention about the coverage status quo, these challenges have sparked a national trend of health systems revisiting their service agreements with anesthesia.
As one of the largest cost centers in a health system, administrators typically look to procedural services for cost reduction opportunities. Successful cost control in perioperative services can have a profound impact on operating margin.4,5 When an anesthesiology group has not been proactive in substantiating their value to key stakeholders, they often find themselves squarely in the crosshairs of hospital administration’s cost reduction efforts, especially if the group receives a subsidy as a part of their services arrangement.
Stipend arrangements within anesthesia service agreements are commonly made to ensure competitive compensation for anesthesia providers given a variety of factors such as an unfavorable payor mix, irregular hours of service, low facility utilization, or administrative duties that may interfere with routine clinical practice. These factors, in addition to other macroeconomic trends, have driven around 80% of hospitals to subsidize the cost of anesthesia services.6
While some of these factors are difficult to change, there are strategies that align incentives between the health system and anesthesia service partners. One model is informally known as a “Cascading Stipend” arrangement. This model functions to reduce the total stipend payout by setting reasonable volume growth goals above a defined baseline, within agreed-upon hours of operation and coverage footprint. Thus, as the hospital grows its volume within a certain time range and fixed coverage footprint, the total subsidy decreases as both parties benefit from marginal case volume and improved productivity.
To implement this model, both parties need to have a robust understanding of the health system’s coverage needs. Historically, this was often modeled using anecdotal experience or pre-built reports with using historical daily averages. Despite sound motivations, these approaches often led to inaccurate predictions. Using historical averages can often result in staffing levels that are either too high or too low, creating sub-optimal coverage and exacerbating tensions between departments.
More recently, advanced analytics tools such as Merlin Heatmap have helped practices visualize where resources are needed by service area, department, day of the week, and time of day. The analytics engine expresses resource demand probabilistically, expediting the creation of accurate staffing models. This helps both the anesthesia group and the hospital system establish ground truth and fine-tune coverage models as new data become available, ensuring resource allocation more closely matches demand.
Figure 1: Operating Room Heatmap Visualization
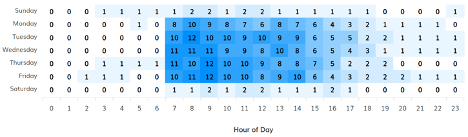
Figure 1. Blue color represents a higher number of concurrent rooms running, white represents a lower number of concurrent rooms running.
The time range of interest for this model typically matches what the hospital would consider “primetime”, which aligns closely with its busiest operating hours. Volume targets are organized into tiers with a defined monetary value. For example, performing 100 cases per year above an agreed-upon baseline during primetime hours would translate to a specific amount “cascaded” off the total stipend amount for the year. So, despite a lower subsidy from the health system, both parties would see improvements in operating margin through increased revenue and a stable cost structure.
Another factor to consider is setting growth targets for different departments in the hospital. Non-procedural areas are growing much more rapidly than more traditional operating room areas, which is a factor both parties should consider before settling on final growth targets.
While this model draws some parallels to a “Collections Guarantee” model, it improves upon that framework by reducing information asymmetry between parties, aligning growth and productivity incentives, and promoting collaboration between the groups as there is mutual benefit from the growth and improved productivity.
Sources
- Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19. American Hospital Association. 2020. https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf
- hospitals are suffering financial damage due to COVID-19 pandemic, Kaufman Hall finds.Healthcare Finance News. 2020. https://www.healthcarefinancenews.com/news/us-hospitals-are-suffering-financial-damage-due-covid-19-pandemic-kaufman-hall-finds
- National trends in nonoperating room anesthesia: procedures, facilities, and patient characteristics. Curr. Opin. Anesthesiology. 2021. https://journals.lww.com/co-anesthesiology/Fulltext/2021/08000/National_trends_in_nonoperating_room_anesthesia_.13.aspx
- Health Sector Economic Indicators – June 2020 Spending Brief.https://altarum.org/sites/default/files/uploaded-publication-files/SHSS-Spending-Brief_June_2020.pdf
- Macario, A. Where Are the Costs in Perioperative Care?https://anesthesiology.pubs.asahq.org/article.aspx?articleid=2323555
- Hospital subsidy support for exclusive anesthesia group practices expected to rise. Becker’s Hospital Review. 2021. https://www.beckershospitalreview.com/hospital-transactions-and-valuation/hospital-subsidy-support-for-exclusive-anesthesia-group-practices-expected-to-rise.html
