1. Establish collaborative governance
A shared governance model will set the stage for collaborative and functional oversight to hardwire safety protocols, provide efficiency gains and enhance volume growth.
Problem: Most hospital ORs are governed by a committee of the medical staff. This committee typically focuses on medical staff dynamics, not organizational performance. The OR nursing director has authority over operations from a nursing perspective, but is not empowered to lead effective change. No leadership body is accountable for the overall performance, inclusive of safety and quality, as well as the strategic success of surgical services. As a result, the OR is a static organization operating in functional silos that lacks the impetus to improve. Ultimately, the OR fails to serve its core customer: surgeons.
Intervention: Create a governance structure that engages all the stakeholders with a vested interest in OR operations — surgeons, anesthesia, nursing and hospital administration.
Leading hospitals have established strong multidisciplinary leadership by creating a Surgical Services Executive Committee. An SSEC is a multidisciplinary “board of directors” for the OR. Members include clinically respected surgeons and anesthesiologists, nursing leaders, hospital senior executives and ad hoc representatives from key ancillary departments. Importantly, the SSEC is sponsored by hospital administration and typically reports to the hospital president and CEO. Because the SSEC is a committee of the hospital (not the medical staff), it is able to focus on the overall performance of the OR. Since the committee includes clinicians, department managers and hospital leaders, it is able to address problems from every angle. It provides a forum to address surgeons’ needs and empowers anesthesia to spearhead operational improvements.
The SSEC’s job is to create a strategic vision for the OR, develop a formal growth strategy, sponsor process improvement and guide cultural change. The SSEC also functions as an operational committee for the surgery department. Members meet frequently to review OR data and address performance problems.
Outcomes: Establishing a multidisciplinary SSEC will set the stage for key improvements in OR operations, financial performance and strategy:
- The SSEC provides a collaborative forum for implementing complex operational improvements, such as improvements in block time allocation, and as a peer-driven entity, creates clear guidelines and transparent processes to manage potentially politically charged issues.
- The SSEC provides oversight of task forces assigned to critical elements within the perioperative service continuum, such as scheduling, pre-surgical testing, OR staffing and safer surgery initiatives. These collaborative initiatives are critical to reducing waste and inefficiency and improving clinical outcomes.
- Ultimately, the SSEC is key to creating a surgeon-focused environment that supports successful market strategy and volume growth.
2. Adopt a single path for surgical scheduling
Optimal scheduling processes help reduce errors and costs related to inefficiency.
Problem: Many hospitals do a poor job of capturing and coordinating patient information prior to surgery. OR schedule requests are received through a variety of routes — phone calls, faxes, emails, written notes and verbal requests. Typically, requests lack full detail on the patient and the procedure. Lack of information creates many opportunities for inefficiency and waste. It also increases the risk of quality problems and adverse patient outcomes.
Intervention: Create a standardized, single-path scheduling system designed to ensure the capture of complete patient and procedure information.
The foundation of an effective scheduling system is a single, standardized process to schedule a case. Typically, a standardized schedule request fax form (accessed online or via an integrated clinic electronic medical record tool) is the answer. A multidisciplinary task force should design the form to capture all the information required to prepare for a case and to identify high-risk patients. Mandatory fields should include complete procedure description information, CPT code, anesthesia requirements, patient comorbidities, patient allergies, testing and preventive care orders and special equipment needs. The elimination of telephonic scheduling in all but urgent/emergent and same-day add-on cases provides for a standardized pathway.
For organizations that primarily utilize facsimile documentation, consider adopting a software solution that digitizes, indexes and stores all incoming faxes to effectively manage documents within the process. Assign nursing staff to review all items upon receipt and sort them into electronic patient folders. The software and associated processes will coordinate scheduling forms, lab reports, imaging reports, consults and other patient documentation. The system ensures that all critical documentation is available as needed and that the patient is fully optimized prior to the day of surgery.
A key part of creating a single-path scheduling system is to develop a “new state map” of the targeted scheduling process. The map should trace the flow of information from the point a case is entered into the system through staff tasks and responsibilities. Case management and discharge planning should also be a parallel component of the scheduling process.
Outcomes: A well-designed single-path scheduling process will reliably capture all the information needed to ensure a safe and efficient surgery.
- Capturing information early — and ensuring a prompt clinical review — prevents many last-minute problems that can lead to case delays and cancellations.
- Reducing delays and cancellations optimizes OR utilization, costs and revenue.
3. Optimize pre-surgical testing
A well designed pre-surgical testing clinic reduces case delays and late cancellations.
Problem: In many hospital surgery departments, pre-surgical preparation is haphazard. Clinical staff do not follow standard protocols for preoperative testing, and preoperative management is poorly coordinated. As a result, many patients arrive on the day of surgery with incomplete tests, incomplete paperwork and unmanaged medical conditions. Ironically, a significant percentage of patients receive excessive testing, leading to high costs. In addition, testing that takes place for elective procedures within 72 hours of surgery are considered bundled in the DRG payment and cannot be compensated separately under CMS payment policy. Patients not optimized prior to surgery have increased risk for greater length of stay, subpar clinical outcomes and underwhelming patient satisfaction.
Intervention: Develop a standardized pre-surgical testing process that ensures all elective surgical patients are evaluated a minimum of three to five business days prior to surgery. The core of an effective process is a set of standard protocols and algorithms — developed under the leadership of anesthesia and hospitalists — for pre-surgical testing and patient management:
- Phone triage. Step one is to develop a risk assessment questionnaire that clinical staff can use to triage patients within 24 hours of being scheduled. Higher-risk patients may be directed to the hospital for an onsite assessment. Often the high-risk assessments are done in conjunction with a hospitalist who may complete the risk assessment and provide guidance for patient preparation.
- Testing matrix. Anesthesia should also develop standard protocols for preoperative testing based on surgical invasiveness and patient comorbid conditions.
- Lab result guidelines. Clinical staff requires guidelines for assessing lab results in a consistent manner and managing abnormal labs.
- Prep protocols. OR leaders should also develop protocols for the preoperative management of patient comorbidities such as diabetes, hypertension and staph aureus screening and preoperative anemia management. Anesthesia should perform a preoperative chart review for all high-risk patients with collaboration with hospitalists. Hospitalists can bill for a level III visit, when appropriate. Hospitalists can assist with pre- and post-surgical patient care to optimize clinical outcomes.
In addition, create an onsite pre-surgical preparation process for coordinating patient information and conducting onsite evaluations of higher-risk patients. Starting at time of surgical scheduling and after a medical record number has been established, clinic staff should actively manage cases to ensure complete patient preparation.
Outcomes: An effective preop process will help OR staff identify and manage patient health issues well ahead of time, ensuring that patients are completely prepared for their surgery. Full patient preparation reduces delays and cancellations. It also has the potential to reduce complications that require additional care and can lead to hospital readmissions, and reduce length of stay. In addition, performing the bulk of elective case pre-surgical testing greater than 72 hours prior to surgery allows the hospital to recoup testing costs through appropriate billing.
4. Institute a document management system for scheduling and PAT
A well designed document management system hardwires both the scheduling and PAT processes to minimize errors in scheduling a case, provides a central repository for patient preoperative information and tracks appropriate information in logical sequence.
Problem: Most hospital systems have highly variable processes for surgical patient intake and patient preparation that are mostly dependent upon judgment of staff and providers versus a standardized process or algorithm. Variability in process creates opportunities for errors, omissions and the potential for adverse patient outcomes.
Intervention: Establish a document tracking system for scheduling and PAT to better orchestrate activities. Systems must be hardwired in place for workflow processes and protocols to be adhered to. Staff require triggering mechanisms for consistent call to action. Standardized processes within scheduling and PAT remove variability and provide consistency in both the service delivery and optimization of patients pre-surgically, improving clinical outcomes.
- Develop an electronic workflow/paperless workflow solution for scheduling and PAT.
- Choose a software solution to convert all faxed communication to electronic documents which are then incorporated into electronic workflows for review, evaluation and acceptance prior to the patient’s scheduled surgery.
- Pre-registration and financial clearance should be incorporated into the process.
- An electronic repository of information improves inter-departmental communication.
- Establish a checks and balance system to ensure the correct procedure is scheduled, the patient is optimized pre-surgically and all clearance is established prior to the day of surgery.
Outcomes: An electronic document management system improves clinical outcomes by hardwiring best practice standards for scheduling, pre-surgical evaluation and testing. Clinical outcomes are improved. Length of stay and costs are reduced. Documentation is enhanced and provides an additional layer of security in identification of the correct procedure, laterality of the procedure and comorbidities.
5. Institute a “daily huddle”
Cross-disciplinary communication improves schedule flow, optimizes resources.
Problem: The processes that lead up to a surgical procedure come together rapidly on the day of surgery. Safe surgery requires fully orchestrated patient information, patient preoperative management, clinical staff, surgical supplies and OR facilities. Problems and issues discovered late in the process can easily lead to a delayed or cancelled case. In addition, last-minute decision-making can lead to waste — the procedure gets done, but not with the most efficient use of resources.
Intervention: Establish a “daily huddle” process to systematically ensure that all the elements of a safe, efficient surgery are in place the day before a procedure.
- The daily huddle is a brief meeting held every day in the early afternoon for the purpose of coordinating the OR schedule.
- The meeting includes representatives from nursing, anesthesia, PAT, scheduling, materials management and other support areas.
- During the daily huddle, participants review current-day problems and schedule issues, then preview cases scheduled for the following day and two to four days forward.
- Clinical staff in the huddle verify that patient charts are complete, all tests have been performed and all health issues have been appropriately managed.
- The daily huddle participants also check the schedule for any anticipated practical problems. Are allotted case times appropriate? Are any special supply requirements in place? Are there any resource conflicts? Are there anticipated delays in day-of-testing requirements that warrant moving the case later in the day? Problematic cases are resolved or rescheduled.
Outcomes: Examining issues from a clinical perspective a day ahead of time enables the OR to prevent many problems on the day of surgery. This reduces cancellations and delays and helps the OR maximize utilization. The daily huddle process can also help the OR avoid potential quality problems that lead to complications, errors, increased length of stay and readmissions.
6. Excellence in sterile processing
Sterile processing can have a dramatic effect on patient safety and clinical outcomes.
Problem: Many hospitals lack the appropriate amount of competent staff, equipment and oversight support required to create a best-performing central sterile processing department. The CSP typically is staffed with uncertified technicians. Core competencies in sterile technique, cleaning, drying and storing are rarely reviewed. CSP is often required to assemble surgical case carts within minimal clinical supervision. The department is typically housed in the lower level of institutions and is not a high priority for senior executives. As a result, instrumentation is not regularly inspected for bioburden which can lead to surgical site infections.
Intervention: Central sterile processing departments require proper support and continuous supervision and supply chain management strategies that address the problem of high costs from multiple angles. Successful ORs use a range of techniques, such as:
- Educate staff. Develop consistent and documented staff education comprised of decontamination of surgical instrument protocols, proper preparation and packaging of instrumentation, proper sterilization of instrumentation, general knowledge of healthcare communication and surgical instruments and the cost/annual spend for surgical instrumentation repairs.
- Dashboards. Develop and publish a departmental dashboard with safety, quality, efficiency, staff productivity and satisfaction indicators. Safety indicators should include percent of trays undergoing immediate sterilization or “flashed,” percent of positive biological and overall surgical site infection rate.
- Reduce flashing. Work with CSP and OR staff to determine the appropriate number of instruments required based upon historical usage. Instrument count and annual spend on instrument repair should be taken into consideration for number of instruments required for the existing case volume. Having an appropriate number of instruments will significantly decrease the flash rate.
Outcomes: Staff education, improved decontamination and sterilization technique and improved oversight will contribute to reduced instrument repair and replacement, reduced surgical site infection and increased OR staff and physician satisfaction.
7. Implement crew resource management
Crew resource management is the glue that holds the group together.
Problem: The lack of a continuous communication loop can contribute to never events, sentinel events and near misses. Root cause analysis of sentinel events indicates that communication is the primary variable in all events.
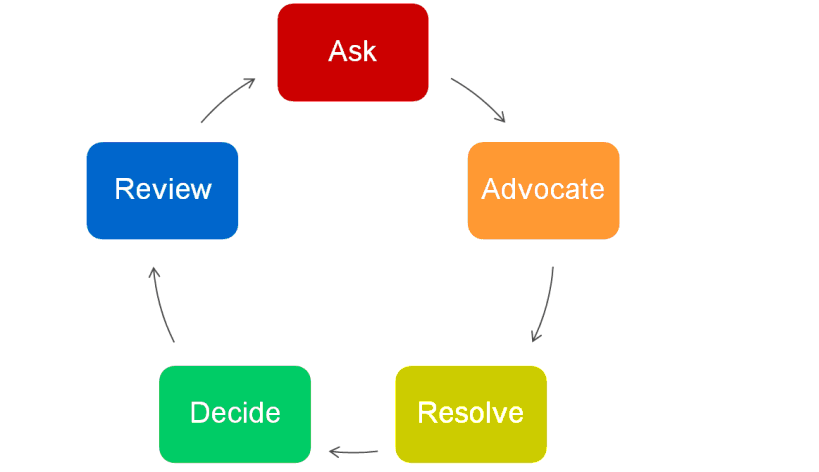
Intervention: Educate staff on team building and proper communication through crew resource management techniques. CRM-trained employees utilize the communication loop depicted in Table 1.
Table 1
- Educate and train OR staff on CRM techniques.
- Emphasize the “advocacy” component of CRM to enhance communication. As an example, one team member doesn’t have a solution to offer but might know of someone else who does or support someone else’s solution. If that is the case then this training teaches individuals to say so and let everyone know where they stand. A statement as simple as, “I understand that you think we need to rush because we are already behind schedule two hours, but I agree with Nurse Jones, let’s just take a minute to make sure we have all the necessary equipment before we begin this procedure since we didn’t plan on doing it this way when it was originally scheduled.”
Outcomes: Trained communication techniques will enhance the content of discussions and provide an additional safety net to reduce never events and improve efficiency, quality, safety and productivity of the department.
8. Implement the WHO safer surgery checklist
A multidisciplinary, collaborative approach to hardwiring safer surgery protocols, inclusive of sign-in, time out and sign-out, checklists can identify where in the process each action should occur.
Problem: Many hospitals struggle with hardwiring protocols to ensure that the number of safety issues, including inadequate anesthetic safety practices, avoidable surgical infection, wrong site surgery and poor communication among team members, are mitigated.
Intervention: The World Alliance established the Safe Surgery Saves Lives initiative for patient safety as part the World Health Organization’s efforts to reduce the number of surgical complications and deaths around the world. The Alliance introduced the concept of using checklists to foster safe patient care and high reliability among medical practitioners. Safety practices are the keys to safe surgical outcomes. The Joint Commission standard definition of safe practices is, “A type of process or structure that, when applied, reduces the probability of adverse events resulting when patients interact with the healthcare system across a range of diseases and procedures.” Checklists contribute directly to the concept of safe outcomes and practices.
- Develop protocols. Develop specific checklists and indicate where in the process each step should occur and by whom. All members of the OR team should be engaged in the development process. The process should not fall solely on nursing, surgeons, technicians or anesthesiologists. Each plays a role and should be engaged in the entire checklist process.
- Accountability. Routine spot checks are required and staff should be empowered to voice concern if steps are missed or not consistently followed in accordance to protocol. Noncompliant surgeons should be counseled and re-educated on the importance of the checklists. Violations in protocol should not be tolerated and should be subject to prescribed medical staff disciplinary actions which ultimately result in revocation of medical staff privileges.
Outcomes: Checklists can reduce never events and near misses, improve clinical outcomes and engrain an overall culture of safety in the department.
9. Ensure that all errors and near misses are recorded
Improvements in safety and quality cannot be made without understanding the root cause of each event.
Problem: Many hospitals cite that their staff are reluctant to report all errors and near misses for fear of retribution or job retention.
Intervention: Establish a “house-wide” protocol for reporting errors and near misses to the appropriate individual. The director of quality and/or risk management should aggregate all data and provide a root cause analysis on all errors and near misses to further refine existing protocols, processes and educational plans.
Outcomes: Improved, transparent communication will result in reduction in errors and near misses. The organization will change to a learning organization striving to improve daily operational activity.
10. Instill a “just culture”
Establishing a “just culture” will afford team members the ability to communicate without fear of retribution and instill a sense of teamwork within their daily work.
Problem: Many hospitals are faced with errors that occur simply due to staff not feeling comfortable voicing concern to physicians or administrators.
Intervention: A “just culture” refers to a way of safety thinking that promotes a questioning attitude, is resistant to complacency, is committed to excellence and fosters both personal accountability and corporate self-regulation in safety matters.
- Establish a learning culture versus a punitive culture.
- Define the border of unacceptable behavior.
- Increase reporting of errors, breakdowns in protocols and identification of trend(s).
- Build trust among team members.
- Establish more effective safety and operational management.
Outcomes: Team member morale and job satisfaction will increase. Never events and near misses will be dramatically reduced if not eradicated.
More Articles on Patient Safety:
Patient Safety Tool: Guide to Reducing Adverse Drug Events
Patient Safety Tool: Surgical Smoke Management Toolkit
Study: Group Learning Can Improve Patient Safety Culture
