There are many areas in the revenue cycle which can disrupt an ASC's revenue stream or cause compliance problems. However, the following are typically the most common to cause difficulties.
1. Coding — This is one area that can affect whether your ASC is receiving the appropriate reimbursement owed. It is important that your coder(s) is certified and ASC-experienced. It's possible that your coder is not coding fully and not coding in synchronization with the provider, including not coding for covered implants, supplies and other services. This reduces the maximum compensation due to the center. Another error coders frequently make is not coding the diagnosis to the highest level of specificity. This can also affect the reimbursement amount.
There are additional problems that may be encountered in coding which are not necessarily directly tied to reimbursement but can affect your center's compliance and may indirectly result in take-backs and possibly fines. These include over-coding, under-coding, unbundling and other types of non-compliance with federal and state regulations.
2. Clean Claims — Delays in prompt and accurate payments often occur because incorrect claims are sent to the clearinghouse and the appropriate member of your billing staff is not printing a clearinghouse report that shows whether the claim was accepted or denied by the payer. Checking this report immediately is paramount because it allows the correction and resubmission of a corrected claim without delay. There should also be a follow up with the payer within 48 hours to determine that the claim is on file to be processed.
3. Follow Up on Denials, Incorrect Payments — It is critical that payer contracts are kept up to date in the software system and that your payment poster is familiar with payer contract requirements. In the event of a notice of non-payment or an incorrect payment, determine the reason for the error and follow up with the payer right away. Respond immediately if the payer is requesting additional information (e.g., operative notes, pathology reports, invoices). It may be helpful to develop payer-specific protocols for handling error resubmissions. If the desired response is not received from the payer, initiate an appeal as necessary.
4. Appeals — Incorrect and non-payment of claims along with contract non-compliance by the payer are the main reasons ASCs initiate an appeal. Lack of timely payments may also be a reason. Understand and enforce your state's prompt payment requirements. Your ASC's collectors and payment posters should be aware of and follow appropriate procedures for the payer's requirements for timely filing of appeals and resubmission of corrected claims. Appeals should be carried to the highest level of adjudication necessary. If progress in the appeal is proceeding slowly, you may need to involve the payer's provider representative and, in some cases, your state's insurance commissioner. Detailed documentation of all phone and e-mail contacts and written correspondence with the payer is important as these records may be required to obtain settlement.
5. Patient Statements — Sending patient statements is a necessary but often overlooked task. It is important that your billing staff submit an initial patient statement immediately upon receiving full and accurate payment from a third-party payer(s). It is then important that a follow-up patient statement is sent every 30 days. Use a tickler file or software program to remind you which patients to bill. This means that you will probably be sending patient statements daily. While a bit cumbersome, this is an easier task than sending all statements at once and maintains a steady reimbursement flow.
Statements should include sequential messages culminating in 90-day final notice. After the final notice, make one more additional attempt to collect the balance by calling the patient and advising them of collection agency intervention and/or encouraging the setting up of a payment plan.
6. Refunds — Although refunds are the reverse of incoming cash flow, they are extremely important for compliance. When a third-party payer or patient refund is indicated, the appropriate billing staff member should promptly complete a refund request outlining the name of the patient, date overpayment received, amount of overpayment and name of person/company to receive the refund. Forward the completed request to the administrator or business office manager to prepare and send an appropriate refund check within 30 days of overpayment
7. Accounts Receivable — Monitoring your ASC's accounts receivable (A/R) is an important part of maintaining a consistent revenue stream. Collectors should understand the different ways to measure A/R to determine delinquent payments by payer and date. These reports also often detect negative third-party payer trends. If a trend is noticed, notify the administrator or business office manager.
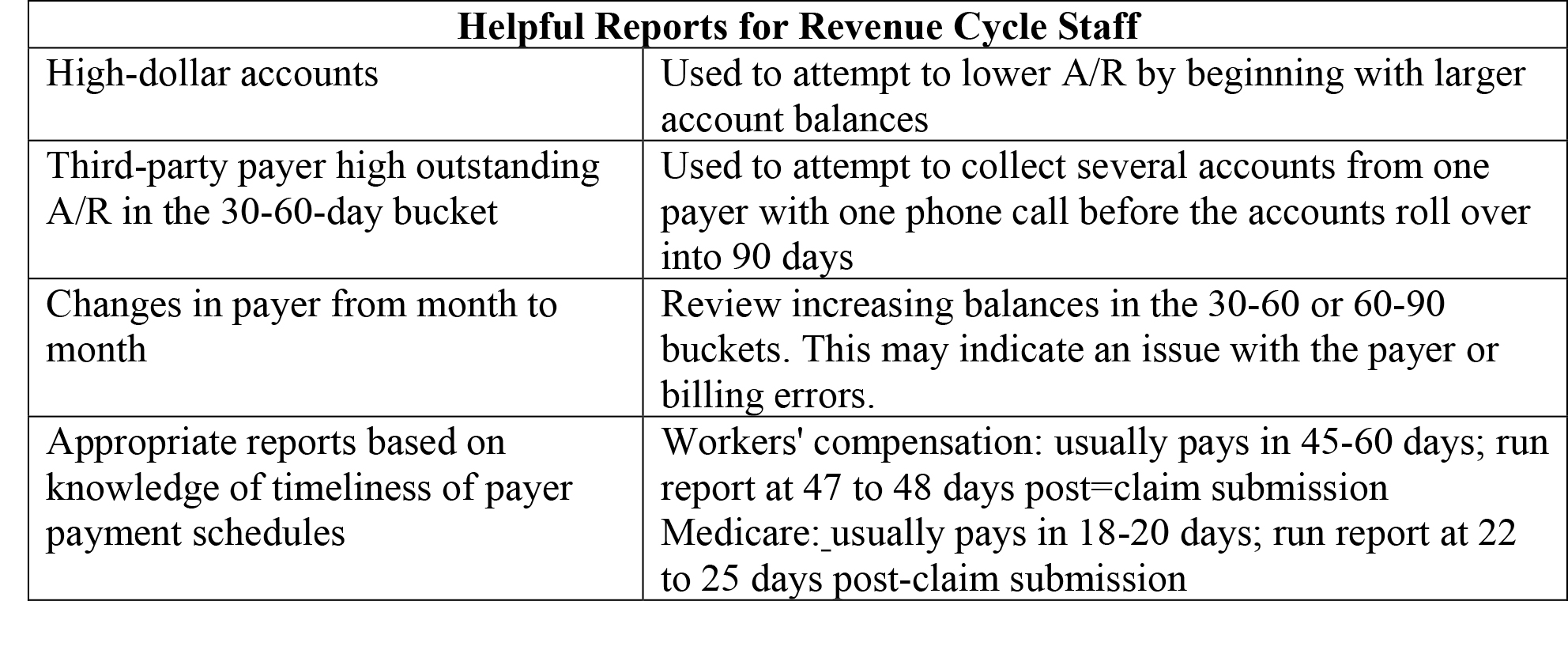
8. Relevant reports: Depending on the software your ASC uses, revenue cycle reports can be generic and perhaps less useful. However, in some ASC-specific software packages, reports can be very specific and measure the financial aspects of your ASC from many angles. End-of-month reporting is important for measuring the success of your billing and collection efforts and comparing them to budgetary goals. The following list illustrates some specialized reports that may be helpful in determining your success in reaching those goals.
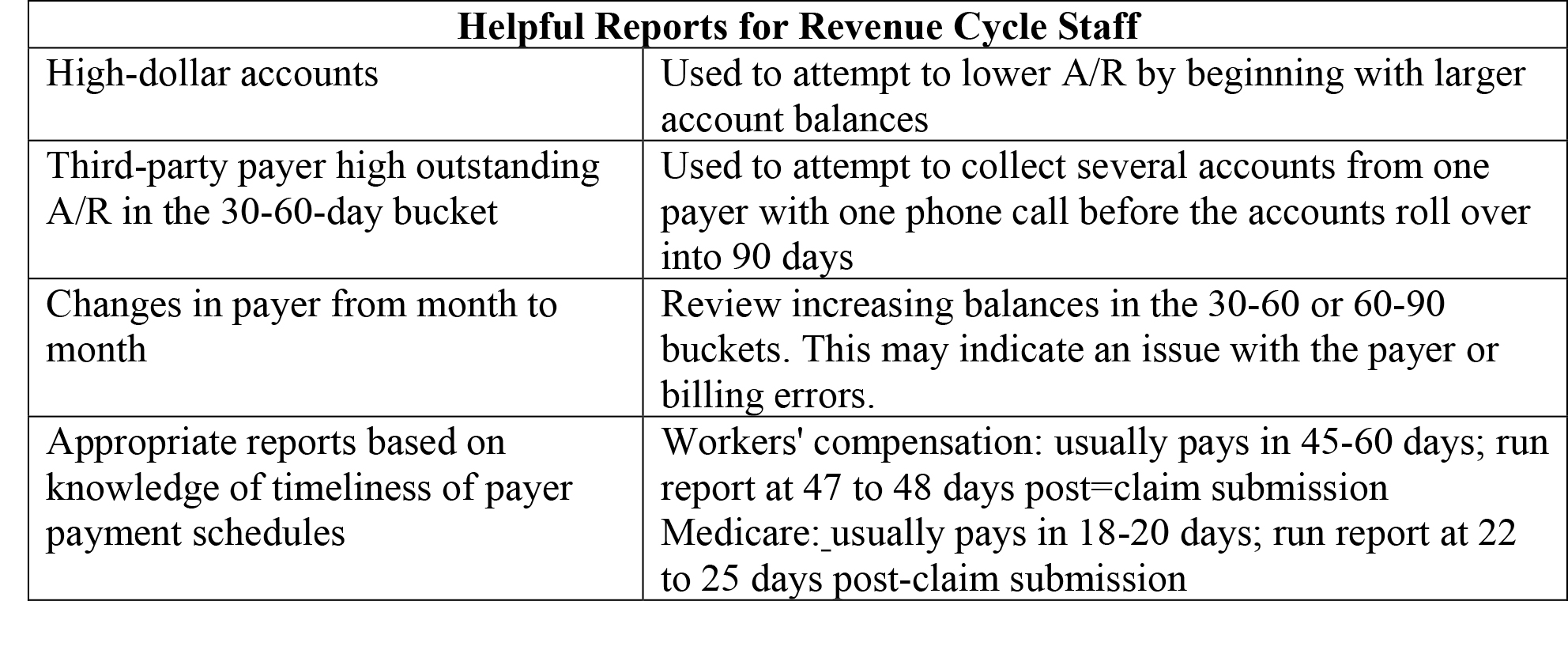
Software-generated reports can be used at any time by your revenue cycle management staff to assist them in collecting monies owed to your ASC. Types of recommended reports and when to run them are as follows:
There are other areas in the revenue cycle that can be problematic. Those described here are just a composite of likely areas to examine for slowdowns in the revenue stream. It is important that a member of your ASC's management team continually audits all areas of the revenue cycle to prevent disruption of your cash flow.
Caryl Serbin, RN, BSN, LHRM, is president and founder of Serbin Medical Billing, an ASC revenue cycle management company. Serbin Medical Billing's primary objectives are to provide the best coding, billing and accounts receivable management services available to ambulatory surgery centers (hospital joint-venture, corporate-owned or independent) and anesthesia providers. Ms. Serbin has been a leader in the ASC industry for 30 years. She was the founder of the first ASC-specific billing company.