According to the Centers for Disease Control and Prevention, surgical site infections account for 17 percent of all nosocomial infections. Of the more than 30 million surgeries performed in the U.S. each year, SSIs occur in approximately 2 to 5 percent of procedures. These types of infections are expensive to treat and consume healthcare resources — one case adds an average of seven to 10 days to a hospital stay and costs between $3,000 and $29,000. In the ambulatory surgery setting, the use of an efficacious, safe, and persistent skin antiseptic such as chlorhexidine gluconate is critically important in order to mitigate risk for development of SSIs.
Some SSIs develop as a result of poor post-operative care of the surgical site, but many are caused by the patient's own microbial flora contaminating the post-operative site as a result of improper skin antisepsis. The role of a skin antiseptic is to remove as much microbial contamination from the patient's skin as possible to reduce the risk for infection. Now more than ever, proper skin antisepsis is a key component of the infection prevention and control process in ambulatory surgery centers.
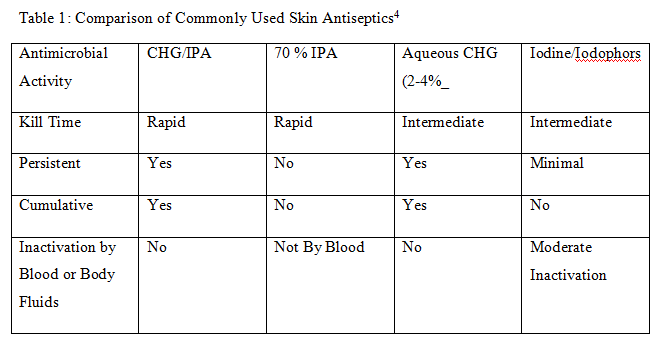
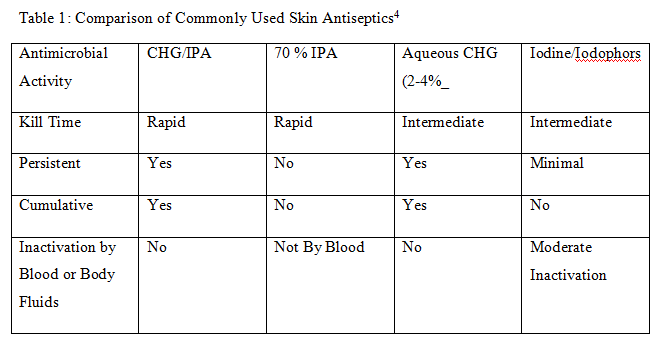
There are many choices for skin antiseptics on the US market including PVP/iodine, isopropyl alcohol, and more recently chlorhexidine gluconate/isopropyl alcohol solutions. According to the Association for Perioperative Registered Nurses Recommended Practices, clinicians should consider a variety of factors when selecting a skin antiseptic including:
• Is the skin antiseptic broad spectrum?
• Is the product quick and easy to use?
• Is the product persistent?
• Will the product maintain its antimicrobial activity in the presence of organic matter, such as blood?
• Is the antiseptic non-irritating to the patient's skin?
In addition, the clinician should carefully consider the most appropriate antiseptic for the patient and the specific procedure.
Chlorhexidine gluconate was first introduced in the U.S. in the 1970s as a hand washing agent for healthcare workers. Since that time, it has been widely used in dental settings, and for the prevention of bloodstream and surgical site infections. Both chlorhexidine gluconate and iodophors have broad spectrum activity against a wide variety of gram positive/gram negative bacteria and pathogenic fungi. When used as preoperative hand scrubs, some comparisons show chlorhexidine gluconate achieved greater reductions in skin microflora than did povidone-iodine and also had greater residual activity after a single application. One of the significant advantages to the use of CHG is the persistent antimicrobial effect of up to seven days with certain concentrations. Persistent antimicrobial activity helps decrease rebound microbial growth after skin preparation. CHG is also not inactivated by blood or body fluids as many other commercially available antiseptics.
The correct use of a skin antiseptic is a key component of the prevention of surgical site infections. Education of the healthcare staff is critical to minimizing risks associated with using any skin antiseptic product. Staff members should be educated on the appropriate indications for use of the product, the application instructions required to effectively inactivate the microorganisms on the product's efficacy label, the material safety data sheet, and the contraindications. Educating the appropriate staff members on the proper use of the chosen product will ensure the manufacturer's documented product efficacy will be achieved and the end users will be protected from adverse reactions.
A consistent approach to providing skin antisepsis combined with staff training, appropriate product usage and education will give healthcare facilities the greatest opportunity to reduce microbial contamination on the patient's skin and will improve healthcare professionals' daily fight against healthcare associated infections. It is also important to not forget the role of hand hygiene. Consistent and proper hand hygiene combined with proper skin antisepsis can have a dramatic effect on reducing the risk for surgical site infections.
For more information on skin antisepsis, visit the Centers for Disease Control and Prevention website at www.cdc.gov or the Association for Perioperative Registered Nurses website at www.aorn.org.
Related Articles on ASC Quality:
Legislation Calls for Unique IDs to Improve Device Safety
Study: Regional Collaboratives Lead to Improved Outcomes, Transparency
Patient Safety Tool: Language Services Toolkit
Some SSIs develop as a result of poor post-operative care of the surgical site, but many are caused by the patient's own microbial flora contaminating the post-operative site as a result of improper skin antisepsis. The role of a skin antiseptic is to remove as much microbial contamination from the patient's skin as possible to reduce the risk for infection. Now more than ever, proper skin antisepsis is a key component of the infection prevention and control process in ambulatory surgery centers.
There are many choices for skin antiseptics on the US market including PVP/iodine, isopropyl alcohol, and more recently chlorhexidine gluconate/isopropyl alcohol solutions. According to the Association for Perioperative Registered Nurses Recommended Practices, clinicians should consider a variety of factors when selecting a skin antiseptic including:
• Is the skin antiseptic broad spectrum?
• Is the product quick and easy to use?
• Is the product persistent?
• Will the product maintain its antimicrobial activity in the presence of organic matter, such as blood?
• Is the antiseptic non-irritating to the patient's skin?
In addition, the clinician should carefully consider the most appropriate antiseptic for the patient and the specific procedure.
Chlorhexidine gluconate was first introduced in the U.S. in the 1970s as a hand washing agent for healthcare workers. Since that time, it has been widely used in dental settings, and for the prevention of bloodstream and surgical site infections. Both chlorhexidine gluconate and iodophors have broad spectrum activity against a wide variety of gram positive/gram negative bacteria and pathogenic fungi. When used as preoperative hand scrubs, some comparisons show chlorhexidine gluconate achieved greater reductions in skin microflora than did povidone-iodine and also had greater residual activity after a single application. One of the significant advantages to the use of CHG is the persistent antimicrobial effect of up to seven days with certain concentrations. Persistent antimicrobial activity helps decrease rebound microbial growth after skin preparation. CHG is also not inactivated by blood or body fluids as many other commercially available antiseptics.
The correct use of a skin antiseptic is a key component of the prevention of surgical site infections. Education of the healthcare staff is critical to minimizing risks associated with using any skin antiseptic product. Staff members should be educated on the appropriate indications for use of the product, the application instructions required to effectively inactivate the microorganisms on the product's efficacy label, the material safety data sheet, and the contraindications. Educating the appropriate staff members on the proper use of the chosen product will ensure the manufacturer's documented product efficacy will be achieved and the end users will be protected from adverse reactions.
A consistent approach to providing skin antisepsis combined with staff training, appropriate product usage and education will give healthcare facilities the greatest opportunity to reduce microbial contamination on the patient's skin and will improve healthcare professionals' daily fight against healthcare associated infections. It is also important to not forget the role of hand hygiene. Consistent and proper hand hygiene combined with proper skin antisepsis can have a dramatic effect on reducing the risk for surgical site infections.
For more information on skin antisepsis, visit the Centers for Disease Control and Prevention website at www.cdc.gov or the Association for Perioperative Registered Nurses website at www.aorn.org.
Related Articles on ASC Quality:
Legislation Calls for Unique IDs to Improve Device Safety
Study: Regional Collaboratives Lead to Improved Outcomes, Transparency
Patient Safety Tool: Language Services Toolkit