Background
Healthcare-associated infections are among the leading causes of preventable prolonged hospital stay and death in the United States. HAIs affect approximately 1.7 million patients, leading to approximately 99,000 deaths and creating $26 billion to $33 billion in excess healthcare costs each year.1 The hands of the healthcare workers are one of the primary mechanisms by which infectious diseases are spread among patients in healthcare institutions.2 Researchers have suggested that individual compliance rates are the most effective means of delivering performance feedback, and according to a study in PLOS ONE, individualized performance feedback doubles the likelihood a healthcare worker will cleanse his hands.3 The increase in hand hygiene is, in part, due to the provision of comprehensive and objective data that helps caregivers understand the reality of their personal and cohort performance.4 Additional advantages of individual feedback include the ability to efficiently allocate human resources, operationalize the rate as part of a fair performance-based educational program and improve caregiver recognition that hand hygiene compliance is his or her personal responsibility.
 Resource allocation, fairness and common sense
Resource allocation, fairness and common sense
From an operational perspective, the value of individual compliance rates falls into two categories. These are the efficient allocation of human resources and fairness, which is the equitable distribution of rewards and corrective action. Efficiency, in this context, could be defined as the use of human resources in the most direct manner to yield the greatest positive change in compliance rates with the smallest amount of effort on the part of managers and infection prevention and quality teams. Fairness would be described as how the front-line caregivers will interpret the level of respect, accuracy and equity in the approach.
The first questions typically asked after receiving a unit-wide aggregate hand hygiene compliance rate are, "What is the next step?" and "How do I operationalize this to improve care at the bedside?" The most common approach would be to share the rate with caregivers on the unit, then begin a process of basic hand hygiene education with all team members. However, in most healthcare organizations there is limited time on both the part of the educator and the healthcare worker. If educators perform basic hand hygiene classes for all unit employees with the intention of improving a 40 percent compliance rate, they are educating both high and low compliers. This is an inefficient allocation of resources.
High performers have the least opportunity to improve the overall unit compliance rate and also represent the lowest risk for the patient. For example, if a high performer has a 97 percent compliance rate, the most she can improve is three compliance points. The small improvement will have only a negligible impact on the aggregate unit rate. In addition, the high performer is by definition already proficient at hand hygiene. This approach can also stress team morale because the high performers are being held accountable (i.e., they are required to attend the hand hygiene classes) because of the poor performance of their non-compliant peers. Many would consider this unfair.
 A more productive, efficient and effective approach would be for managers to focus educational resources on low compliers, and especially individuals with high frequencies of patient contact. This is most beneficial for the patient because a low complier will have a greater opportunity to put the patient at risk than will someone whose individual compliance rate is very high. For example, increasing hand hygiene adherence of a caregiver with 23 percent compliance and 400 patient interactions would have a much greater potential impact on patient safety than increasing the hand hygiene of a caregiver with 97 percent compliance and only 50 patient interactions.
A more productive, efficient and effective approach would be for managers to focus educational resources on low compliers, and especially individuals with high frequencies of patient contact. This is most beneficial for the patient because a low complier will have a greater opportunity to put the patient at risk than will someone whose individual compliance rate is very high. For example, increasing hand hygiene adherence of a caregiver with 23 percent compliance and 400 patient interactions would have a much greater potential impact on patient safety than increasing the hand hygiene of a caregiver with 97 percent compliance and only 50 patient interactions.
This educational method is impossible without detailed insight to individual performance. Based on this type of evaluation, managers of one 31-bed adult medical-surgical unit focused on educating six patient care technicians with low compliance and high patient contact. When comparing the weeks before and after education, individual compliance rates rose from between 27.8 percent to 481.1 percent, and the unit compliance rate rose by 36.3 percent. Since that time, the PCTs have maintained very high compliance scores, consistently exceeding 95 percent. By applying caregiver-specific data, managers can direct limited resources to the areas of greatest need and quickly impact unit performance.
Other common strategies used in the absence of caregiver-specific rates include positive reinforcement in the form of non-monetary awards, gift certificates, recognition in team meetings and financial incentives based on performance evaluations. Individual compliance rates are more effective for ensuring that rewards are directed toward those individuals who are performing at acceptable levels. An equitable distribution of positive reinforcement will enhance team perception of the fairness of the reward program. The goal is to reward desired performance. Common team rewards for aggregate improvements (such as unit pizza parties) reward both high and low compliers to an equal degree. Unit recognitions that benefit the low compliers to the same degree as high compliers do not appeal to a common sense of fair play.
Individual feedback in an aggregate rate environment
Confronting others with constructive criticism and feedback in order to hold them respectfully accountable for their actions and behavior is an important leadership skill.5 In the absence of individual compliance rates, the only way to provide individual performance feedback is to directly observe and approach caregivers when they are non-compliant. There have been many creative approaches to direct observation and feedback including the presentation of "tickets" to caregivers when they are seen not washing their hands. With this approach, a copy of the ticket is sent to the person's director, manager or department head, and another copy is sent to the infection prevention department. Additional education is provided with each ticket, and consequences increase as well (for example, verbal warnings, written warnings, letters from the peer review committee, culminating in possible termination after five tickets).6
While the purveyors of this approach were well-intended and reported some success, there are difficulties inherent in the execution of such a strategy. The presentation of a "ticket" can be challenging and embarrassing for both the observer/educator and the person committing the infraction, since these interactions often occur on the nursing unit in view and/or hearing of patients, visitors and co-workers. Also, issuing a fifth termination-triggering "ticket" for the final non-compliant hand hygiene opportunity would most likely not be an enjoyable experience. It is difficult to make these conversations objective and emotionally painless for both parties and there may be concerns about the employee's potential negative reactions (e.g., hurt feelings, anger, defensiveness, violence, verbal threats, retaliation, etc.).7 This approach not only burdens the observer with conducting personnel management activities with caregivers who may not report directly to them, it also strains inter-departmental relationships and reduces trust and cross-functional cooperation. Additionally, the infection preventionist (or other observer), who should be seen as an important resource for information and guidance, is now perceived as a threat rather than a collaborative member of the care delivery team.
Systematic approaches for constructive feedback, including clear and well-articulated expectations along with follow-up and recognition in a timely manner, are recommended to reduce conflict and increase accountability.8 Measuring hand hygiene over time and over many caregiver-patient interactions provides a reasonable, unbiased and objective measure on which to base a progressive system of discipline. Using electronic monitoring, a registered nurse routinely compiles over 2,000 patient interactions per month. Just washing in and washing out results in at least 4,000 hand hygiene opportunities.
In the "ticket" approach described above, the trigger for the possible termination of a caregiver's employment would be five non-compliant observations. For 4,000 hand hygiene opportunities, five infractions would represent only 0.00125 percent of the total activity performed by the caregiver. This is an insignificant basis upon which to terminate a healthcare worker's employment, especially considering that a caregiver with a 95 percent compliance rate will be noncompliant 200 times in 4,000 opportunities. While consistently encouraging adherence to protocol, we recognize that there are many reasons that could contribute to periodic episodes of non-compliance. Chronically non-adherent staff may need more attention, with possible disciplinary action, to motivate changes in behavior.6 Situations such as continued and/or blatant disregard for established patient and employee safety policies must be addressed.
Ultimately, accountability is in the employee's (and patient's) best interest and employees tend to respect supervisors who hold them accountable. Being specific in describing the behavior is the most important rule in giving feedback to others.9 Individual hand hygiene compliance rates reflecting the employee's comprehensive performance provide the objective measure to accurately determine an established pattern of behavior, which then gives the manager the information necessary to make a fair assessment and a fully informed decision. Fortunately, these situations represent the minority of noncompliance. In most instances clear, accurate and specific feedback on expectations and performance are effective in motivating well-meaning healthcare providers to increase their hand hygiene adherence.
 Success with individual compliance rates
Success with individual compliance rates
The power of peer-visible individual compliance rates can be illustrated in a 254-bed short-term acute-care facility we work with. On one 12-bed adult medical-surgical critical care ward, 104 caregivers were anonymously assigned badges designated Nurse 1, Nurse 2, etc. Working with local union representatives, the team later decided to monitor caregiver performance by name then identify and post compliance rates. Hand hygiene compliance increased 40.2 percent when comparing pre- and post-identification periods.
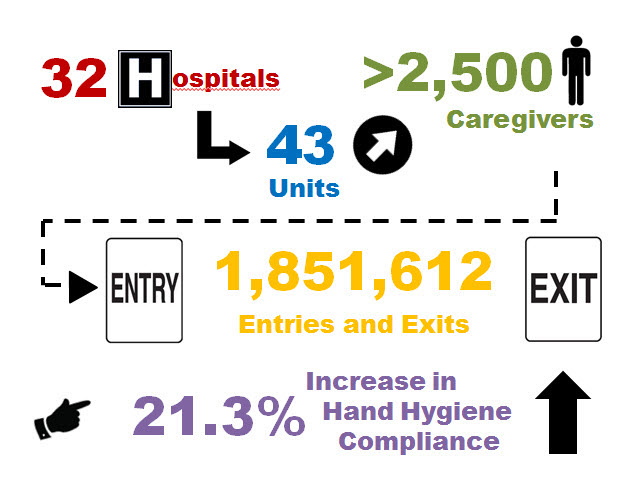
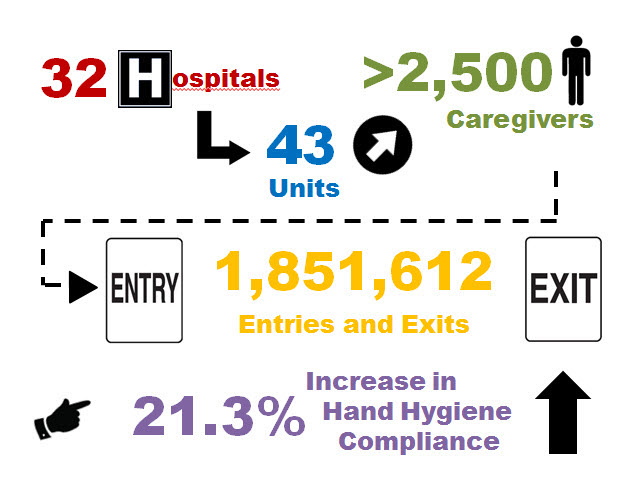
Results for this site were consistent with those seen in a broader analysis of 18 adult critical care wards and 31 adult medical-surgical wards across 32 U.S. hospitals we work with. This analysis included over 2,500 clinical and non-clinical healthcare workers and 1,851,612 caregiver patient room entries, exits and associated hand cleansings. Beginning in October 2012, teams at these 32 facilities began using themed hand hygiene reports to increase feedback to participants and stimulate peer competition. Caregivers received current individual performance rates at electronic communications unit screens located above each dispenser. Efforts included posting individual and unit compliance rates, tips for improvement, progress toward unit goals and recognition of top compliers. Open display of individual compliance rates leveraged the peer expectation that to be an accepted member of the group, everyone would be expected to participate in order to attain the team's goal. Presentation formats were updated weekly with engaging cultural and holiday themes. Caregiver feedback was overwhelmingly positive and the aggregate hand hygiene compliance rate across these sites increased significantly by 21.3 percent (Student's t-test, paired t 3.468 (48), p = 0.0011, SAS) in the first month of the campaign.
Conclusion
Accurate, frequent and comprehensive individual performance feedback is critical to motivating higher performance. The advantages include the ability to efficiently allocate human resources, the ability to operationalize the rate as part of a fair and equitable behavior modification program and enhanced caregiver recognition that hand hygiene compliance is his or her personal responsibility. Methodical application of caregiver-specific performance data has resulted in hand hygiene improvements in more than 30 hospitals across the U.S.
David Sellers is vice president of clinical research at Proventix Systems, a healthcare technology company based in Birmingham, Ala., that produces nGage, an electronic hand hygiene monitoring system. As a registered nurse, former public health advisor for the Centers for Disease Control and Prevention, infection preventionist and hospital COO, Mr. Sellers has 23 years of healthcare experience and insight.
Elizabeth Pembleton is a Clinical Services Analyst at Proventix Systems. She has a diverse background in Public Health with a Bachelor of Science in Health Promotion and Behavior and a Master of Public Health in Epidemiology. She has worked as a behavioral interventionist in hospital, governmental, and non-profit sectors and has completed research in the field of infectious diseases.
References
1 Healthcare-associated Infections (HAI). (2012). Retrieved May 30, 2012, from Centers for Disease Control and Prevention: www.cdc.gov/hai/
2 Aboumatar, H, Ristaino P, Davis R, Thompson C, Maragakis L, Cosgrove S, Rosenstein B, Perl T. (2012) Infection prevention promotion program based on the PRECEDE model: improving hand hygiene behaviors among healthcare personnel. Infect Control Hosp Epidemiol.33(2):144-151.
3 Fuller C, Michie S, Savage J, McAteer J, Besser S, et al. (2012). The Feedback Intervention Trial (FIT) — Improving Hand-Hygiene Compliance in UK Healthcare Workers: A Stepped Wedge Cluster Randomised Controlled Trial. PLoS ONE 7(10): e41617. doi:10.1371/journal.pone.0041617
4 Ontario, Canada, Ministry of Health and Long-Term Care: A Quick Guide to Just Clean Your Hands: A Provincial Hand Hygiene Improvement Program for Hospitals. 2008. http://www.justcleanyourhands.ca/pdf/14_5_A Quick_Guide.pdf. Accessed April 10, 2013.
5 Bandura, A. (1986). Differential engagement of self-reactive influences in cognitive motivation. Organizational Behavior and Human Decision Processes, 38(1), 92-113.
6 The Joint Commission. (2009). Measuring Hand Hygiene Adherence: Overcoming the Challenges, Hand Hygiene Monograph, 115.
7 Harris, G. (2010). Retrieved April 10, 2013. How to Inspire Workplace Behaviors To Get Better Results. Executive Leadership Coaching.
8 Hoover, J. & DiSilvestro, R. (2005). The Art of Constructive Confrontation. Hoboken, NJ: John Wiley & Sons.
9 Karp, H. (1987). The Lost Art of Feedback. The 1987 Annual: Developing Human Resources. San Diego, CA: University Associates, Inc.
Healthcare-associated infections are among the leading causes of preventable prolonged hospital stay and death in the United States. HAIs affect approximately 1.7 million patients, leading to approximately 99,000 deaths and creating $26 billion to $33 billion in excess healthcare costs each year.1 The hands of the healthcare workers are one of the primary mechanisms by which infectious diseases are spread among patients in healthcare institutions.2 Researchers have suggested that individual compliance rates are the most effective means of delivering performance feedback, and according to a study in PLOS ONE, individualized performance feedback doubles the likelihood a healthcare worker will cleanse his hands.3 The increase in hand hygiene is, in part, due to the provision of comprehensive and objective data that helps caregivers understand the reality of their personal and cohort performance.4 Additional advantages of individual feedback include the ability to efficiently allocate human resources, operationalize the rate as part of a fair performance-based educational program and improve caregiver recognition that hand hygiene compliance is his or her personal responsibility.
 Resource allocation, fairness and common sense
Resource allocation, fairness and common senseFrom an operational perspective, the value of individual compliance rates falls into two categories. These are the efficient allocation of human resources and fairness, which is the equitable distribution of rewards and corrective action. Efficiency, in this context, could be defined as the use of human resources in the most direct manner to yield the greatest positive change in compliance rates with the smallest amount of effort on the part of managers and infection prevention and quality teams. Fairness would be described as how the front-line caregivers will interpret the level of respect, accuracy and equity in the approach.
The first questions typically asked after receiving a unit-wide aggregate hand hygiene compliance rate are, "What is the next step?" and "How do I operationalize this to improve care at the bedside?" The most common approach would be to share the rate with caregivers on the unit, then begin a process of basic hand hygiene education with all team members. However, in most healthcare organizations there is limited time on both the part of the educator and the healthcare worker. If educators perform basic hand hygiene classes for all unit employees with the intention of improving a 40 percent compliance rate, they are educating both high and low compliers. This is an inefficient allocation of resources.
High performers have the least opportunity to improve the overall unit compliance rate and also represent the lowest risk for the patient. For example, if a high performer has a 97 percent compliance rate, the most she can improve is three compliance points. The small improvement will have only a negligible impact on the aggregate unit rate. In addition, the high performer is by definition already proficient at hand hygiene. This approach can also stress team morale because the high performers are being held accountable (i.e., they are required to attend the hand hygiene classes) because of the poor performance of their non-compliant peers. Many would consider this unfair.
 A more productive, efficient and effective approach would be for managers to focus educational resources on low compliers, and especially individuals with high frequencies of patient contact. This is most beneficial for the patient because a low complier will have a greater opportunity to put the patient at risk than will someone whose individual compliance rate is very high. For example, increasing hand hygiene adherence of a caregiver with 23 percent compliance and 400 patient interactions would have a much greater potential impact on patient safety than increasing the hand hygiene of a caregiver with 97 percent compliance and only 50 patient interactions.
A more productive, efficient and effective approach would be for managers to focus educational resources on low compliers, and especially individuals with high frequencies of patient contact. This is most beneficial for the patient because a low complier will have a greater opportunity to put the patient at risk than will someone whose individual compliance rate is very high. For example, increasing hand hygiene adherence of a caregiver with 23 percent compliance and 400 patient interactions would have a much greater potential impact on patient safety than increasing the hand hygiene of a caregiver with 97 percent compliance and only 50 patient interactions. This educational method is impossible without detailed insight to individual performance. Based on this type of evaluation, managers of one 31-bed adult medical-surgical unit focused on educating six patient care technicians with low compliance and high patient contact. When comparing the weeks before and after education, individual compliance rates rose from between 27.8 percent to 481.1 percent, and the unit compliance rate rose by 36.3 percent. Since that time, the PCTs have maintained very high compliance scores, consistently exceeding 95 percent. By applying caregiver-specific data, managers can direct limited resources to the areas of greatest need and quickly impact unit performance.
Other common strategies used in the absence of caregiver-specific rates include positive reinforcement in the form of non-monetary awards, gift certificates, recognition in team meetings and financial incentives based on performance evaluations. Individual compliance rates are more effective for ensuring that rewards are directed toward those individuals who are performing at acceptable levels. An equitable distribution of positive reinforcement will enhance team perception of the fairness of the reward program. The goal is to reward desired performance. Common team rewards for aggregate improvements (such as unit pizza parties) reward both high and low compliers to an equal degree. Unit recognitions that benefit the low compliers to the same degree as high compliers do not appeal to a common sense of fair play.
Individual feedback in an aggregate rate environment
Confronting others with constructive criticism and feedback in order to hold them respectfully accountable for their actions and behavior is an important leadership skill.5 In the absence of individual compliance rates, the only way to provide individual performance feedback is to directly observe and approach caregivers when they are non-compliant. There have been many creative approaches to direct observation and feedback including the presentation of "tickets" to caregivers when they are seen not washing their hands. With this approach, a copy of the ticket is sent to the person's director, manager or department head, and another copy is sent to the infection prevention department. Additional education is provided with each ticket, and consequences increase as well (for example, verbal warnings, written warnings, letters from the peer review committee, culminating in possible termination after five tickets).6
While the purveyors of this approach were well-intended and reported some success, there are difficulties inherent in the execution of such a strategy. The presentation of a "ticket" can be challenging and embarrassing for both the observer/educator and the person committing the infraction, since these interactions often occur on the nursing unit in view and/or hearing of patients, visitors and co-workers. Also, issuing a fifth termination-triggering "ticket" for the final non-compliant hand hygiene opportunity would most likely not be an enjoyable experience. It is difficult to make these conversations objective and emotionally painless for both parties and there may be concerns about the employee's potential negative reactions (e.g., hurt feelings, anger, defensiveness, violence, verbal threats, retaliation, etc.).7 This approach not only burdens the observer with conducting personnel management activities with caregivers who may not report directly to them, it also strains inter-departmental relationships and reduces trust and cross-functional cooperation. Additionally, the infection preventionist (or other observer), who should be seen as an important resource for information and guidance, is now perceived as a threat rather than a collaborative member of the care delivery team.
Systematic approaches for constructive feedback, including clear and well-articulated expectations along with follow-up and recognition in a timely manner, are recommended to reduce conflict and increase accountability.8 Measuring hand hygiene over time and over many caregiver-patient interactions provides a reasonable, unbiased and objective measure on which to base a progressive system of discipline. Using electronic monitoring, a registered nurse routinely compiles over 2,000 patient interactions per month. Just washing in and washing out results in at least 4,000 hand hygiene opportunities.
In the "ticket" approach described above, the trigger for the possible termination of a caregiver's employment would be five non-compliant observations. For 4,000 hand hygiene opportunities, five infractions would represent only 0.00125 percent of the total activity performed by the caregiver. This is an insignificant basis upon which to terminate a healthcare worker's employment, especially considering that a caregiver with a 95 percent compliance rate will be noncompliant 200 times in 4,000 opportunities. While consistently encouraging adherence to protocol, we recognize that there are many reasons that could contribute to periodic episodes of non-compliance. Chronically non-adherent staff may need more attention, with possible disciplinary action, to motivate changes in behavior.6 Situations such as continued and/or blatant disregard for established patient and employee safety policies must be addressed.
Ultimately, accountability is in the employee's (and patient's) best interest and employees tend to respect supervisors who hold them accountable. Being specific in describing the behavior is the most important rule in giving feedback to others.9 Individual hand hygiene compliance rates reflecting the employee's comprehensive performance provide the objective measure to accurately determine an established pattern of behavior, which then gives the manager the information necessary to make a fair assessment and a fully informed decision. Fortunately, these situations represent the minority of noncompliance. In most instances clear, accurate and specific feedback on expectations and performance are effective in motivating well-meaning healthcare providers to increase their hand hygiene adherence.
 Success with individual compliance rates
Success with individual compliance rates The power of peer-visible individual compliance rates can be illustrated in a 254-bed short-term acute-care facility we work with. On one 12-bed adult medical-surgical critical care ward, 104 caregivers were anonymously assigned badges designated Nurse 1, Nurse 2, etc. Working with local union representatives, the team later decided to monitor caregiver performance by name then identify and post compliance rates. Hand hygiene compliance increased 40.2 percent when comparing pre- and post-identification periods.
Results for this site were consistent with those seen in a broader analysis of 18 adult critical care wards and 31 adult medical-surgical wards across 32 U.S. hospitals we work with. This analysis included over 2,500 clinical and non-clinical healthcare workers and 1,851,612 caregiver patient room entries, exits and associated hand cleansings. Beginning in October 2012, teams at these 32 facilities began using themed hand hygiene reports to increase feedback to participants and stimulate peer competition. Caregivers received current individual performance rates at electronic communications unit screens located above each dispenser. Efforts included posting individual and unit compliance rates, tips for improvement, progress toward unit goals and recognition of top compliers. Open display of individual compliance rates leveraged the peer expectation that to be an accepted member of the group, everyone would be expected to participate in order to attain the team's goal. Presentation formats were updated weekly with engaging cultural and holiday themes. Caregiver feedback was overwhelmingly positive and the aggregate hand hygiene compliance rate across these sites increased significantly by 21.3 percent (Student's t-test, paired t 3.468 (48), p = 0.0011, SAS) in the first month of the campaign.
Conclusion
Accurate, frequent and comprehensive individual performance feedback is critical to motivating higher performance. The advantages include the ability to efficiently allocate human resources, the ability to operationalize the rate as part of a fair and equitable behavior modification program and enhanced caregiver recognition that hand hygiene compliance is his or her personal responsibility. Methodical application of caregiver-specific performance data has resulted in hand hygiene improvements in more than 30 hospitals across the U.S.
David Sellers is vice president of clinical research at Proventix Systems, a healthcare technology company based in Birmingham, Ala., that produces nGage, an electronic hand hygiene monitoring system. As a registered nurse, former public health advisor for the Centers for Disease Control and Prevention, infection preventionist and hospital COO, Mr. Sellers has 23 years of healthcare experience and insight.
Elizabeth Pembleton is a Clinical Services Analyst at Proventix Systems. She has a diverse background in Public Health with a Bachelor of Science in Health Promotion and Behavior and a Master of Public Health in Epidemiology. She has worked as a behavioral interventionist in hospital, governmental, and non-profit sectors and has completed research in the field of infectious diseases.
References
1 Healthcare-associated Infections (HAI). (2012). Retrieved May 30, 2012, from Centers for Disease Control and Prevention: www.cdc.gov/hai/
2 Aboumatar, H, Ristaino P, Davis R, Thompson C, Maragakis L, Cosgrove S, Rosenstein B, Perl T. (2012) Infection prevention promotion program based on the PRECEDE model: improving hand hygiene behaviors among healthcare personnel. Infect Control Hosp Epidemiol.33(2):144-151.
3 Fuller C, Michie S, Savage J, McAteer J, Besser S, et al. (2012). The Feedback Intervention Trial (FIT) — Improving Hand-Hygiene Compliance in UK Healthcare Workers: A Stepped Wedge Cluster Randomised Controlled Trial. PLoS ONE 7(10): e41617. doi:10.1371/journal.pone.0041617
4 Ontario, Canada, Ministry of Health and Long-Term Care: A Quick Guide to Just Clean Your Hands: A Provincial Hand Hygiene Improvement Program for Hospitals. 2008. http://www.justcleanyourhands.ca/pdf/14_5_A Quick_Guide.pdf. Accessed April 10, 2013.
5 Bandura, A. (1986). Differential engagement of self-reactive influences in cognitive motivation. Organizational Behavior and Human Decision Processes, 38(1), 92-113.
6 The Joint Commission. (2009). Measuring Hand Hygiene Adherence: Overcoming the Challenges, Hand Hygiene Monograph, 115.
7 Harris, G. (2010). Retrieved April 10, 2013. How to Inspire Workplace Behaviors To Get Better Results. Executive Leadership Coaching.
8 Hoover, J. & DiSilvestro, R. (2005). The Art of Constructive Confrontation. Hoboken, NJ: John Wiley & Sons.
9 Karp, H. (1987). The Lost Art of Feedback. The 1987 Annual: Developing Human Resources. San Diego, CA: University Associates, Inc.

