In a Dec. 6 webinar hosted by Becker's Healthcare, Linda Lansing, senior vice president of clinical services, and Kelly Bemis, director of clinical services at Surgical Care Affiliates, discussed implementing a safe surgery checklist at a surgery center.
History & justification for checklists
Ms. Lansing began the webinar with an overview of the history of the surgical checklist. "If you look at the literature, you'll see that the development of checklists from a professional point of view ties back to the aviation industry — and, most significantly, to the aviation industry during the 1930s and 40s," she said. During that time, airplanes were gaining more sophisticated technology in the cockpit, causing problems for pilots who had previously operated more simple machines. Though the technology was intended to improve safety, it was widely considered "too complicated" for a pilot to manage. The number of crashes during this time period attested to the high error rate.
In examining the behavior of pilots in these new planes, experts found that the pilots with the most flying experience were not always the ones with the best results. "We usually think that time and grade in a profession will go ahead and give us competence, and competence will drive … safety and good quality results," Ms. Lansing said. But the human brain is flawed, and even the best training does not prevent a pilot from forgetting a crucial task for take-off.
"They really began to consider: How do you deal with extreme complexity?" Ms. Lansing said. "How do you ensure you complete every step in the process, particularly when that process is done very frequently?" Interestingly, the more frequent and routine a process was, the more likely errors were to occur. As it turns out, when you've performed the same task a hundred times, you fall into a certain sense of complacency about double-checking your work.
To ensure that pilots didn't forget crucial steps, the aviation industry developed a series of checklists. At first, they were used as a memory aid: The pilot would go through and complete every activity, then refer to the checklist to make sure everything was done. It was eventually determined that a more effective approach was to go through the checklist step-by-step, reading each task out loud and attending to issues as they arose.
Why are checklists difficult to implement?
Atul Gawande is an American surgeon and journalist whose books include Better, Complications, and — most relevant to this subject — The Checklist Manifesto. He has advocated heavily for surgical checklists, arguing that the fallibility of human memory opens the door for serious, fatal errors when surgeons rely on their training alone.
Ms. Lansing said part of the difficulty in implementing checklists comes down to an attitude of individual autonomy in medicine. Surgeons, who have gone through years of training, often believe that good medicine is up to the talents of an individual physician — not the collective, systematic effort of a checklist. But studies have proven that checklists vastly reduce the incidence of surgical errors, so the question becomes not, "Should we implement a checklist?" but, "How do we do it?"
Ms. Lansing said team members should follow a "professional code of conduct," with three key characteristics:
• Selflessness. Surgeons and team members must put the needs of others above their own. This eliminates feelings of personal pride over using a checklist or double-checking with others.
• Strong skillset. Surgeons and team members must be well-trained in their field and able to execute tasks well.
• Trustworthiness. Surgeons and team members must be responsible for their personal behavior with others and present themselves as team players.
Dr. Gawande said airline pilots take this a step further. They add a fourth dimension: discipline. "They really feel it's part of being a professional to follow prudent procedures when working with others, because it's important that everyone involved in a process or procedure is operating in the same way," Ms. Lansing said. This idea is in stark contrast to the image of the maverick surgeon, but you can't argue with the results: Study after study says that it works.
"If you think about medicine, we have a tendency to place a great deal of value on autonomy," Ms. Lansing said. "We want to be autonomous and make individual assessments. [Dr. Gawande] challenges that that is actually… in direct opposition to discipline. Is it right and professional to put the needs of autonomy in front of the need for discipline?"
Medicare and accreditation requirements
Ms. Lansing turned the floor over to Ms. Bemis to discuss regulatory requirements for surgical checklists.
Last year, Medicare announced that ASCs would be required to start quality reporting in 2012. In addition to reporting the use of safe surgery checklists, surgery centers are required to perform quality metric reporting using G-codes, reporting whether patients have had transfers, falls, burns and other issues. While these metrics only apply to Medicare patients, the safe surgery checklist must be used on all surgical patients, and ASCs must report they used it for all payors.
For 2012, the initial year of data collection, ASCs may report "yes" if they used it during any part of the year. That means that if you haven't started yet, there's still time. In subsequent years, the ASC will have to use the checklist for the entire year to answer "yes."
ASC leaders will report their surgical checklist use on a secure area of the QualityNet website starting July 1, 2013 and ending Aug. 15, 2013. CMS does not provide a required form for the surgical checklist, so surgery centers can tweak the items to best fit their needs. "This helps to increase the likelihood of compliance," Ms. Bemis said.
CMS is not planning to include the use of the safe surgery checklist in its surveys, and no financial penalties will be incurred at this time. "But that could change — and it frequently does," Ms. Bemis said.
The Medicare requirements target safe surgery practices during three critical periods:
• Prior to anesthesia, including marking the site, identifying the patient, identifying allergies and airway issues, etc.
• Prior to incision, including the time-out process, the timely administration of antibiotics, etc.
• Prior to the patient leaving the OR, including debriefing, identifying concerns that arose in the operating room, etc.
"When we think about Conditions for Coverage requirements, they're really looking for the use of standardized procedures to avoid errors," Ms. Bemis said. "They want to see that you have a pre-procedure verification process to ensure all relevant documents and related information is available and correctly identified."
Accreditation requirements
Accreditation requirements vary slightly from CMS requirements, with slight differences between different accrediting bodies. The Joint Commission developed and publicized the use of a standardized checklist in 2003, later deciding to convert the checklist to universal protocol. The Joint Commission requires that ASCs:
• Conduct a pre-procedure verification process. This means making sure you have the correct procedure, patient and site and identifying that all items necessary for the procedure are present.
• Mark the procedure site. Use an unambiguous and consistent mark to identify the procedure site.
• Perform a time-out immediately prior to starting the procedure.
The Joint Commission has aligned its universal protocol with CMS requirements for a safe surgery checklist.
The requirements for AAAHC accreditation are slightly different again. The AAAHC requires that ASCs:
• Utilize a process involving the patient to identify and designate surgical procedure and surgical site
• Have the OR manager verify site, identity, procedure and that all equipment is available immediately prior to beginning the procedure
"There is a thread of similarities between organizations," Ms. Bemis said. She added that there are several sample checklists that ASCs can use or tweak as needed. One checklist comes from the World Health Organization and is divided into three components that reflect the original Medicare requirements. Another sample checklist, developed by AORN, has taken items from WHO and also considered items in regard to national patient safety goals. The AORN list is divided into four areas: pre-procedure check-in, sign-in, time-out and sign-out.
For any checklist, the key is simplicity. "An overly detailed checklist can became so unwieldy that it isn't used and actually gets in the way of getting things done," Ms. Bemis said.
Development and implementation: A checklist for using checklists
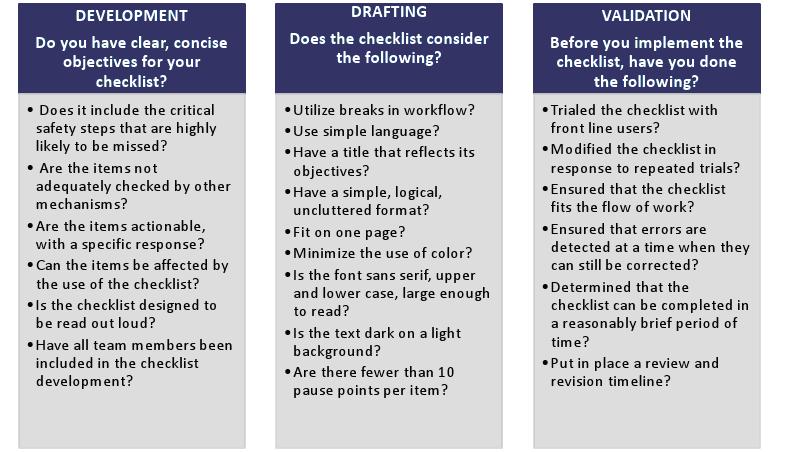
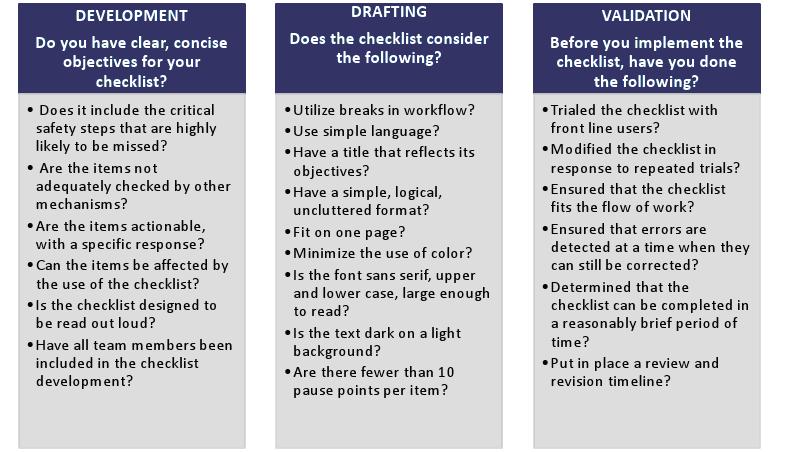
Ms. Lanisng showed the following list of ideas to implement a surgical checklist. This guideline for checklist format and structure was developed by Dr. Gawande and can be found in his book.
In order to implement a safe surgery checklist, she said four key components are crucial.
1. Engage actively with key stakeholders. Your key stakeholders in this situation are OR teammates and physicians, and everyone needs to work together to make a checklist effective. "If we have a lack of engagement in development of the checklist, that's the number one reason for poor follow-through," Ms. Bemis said.
Make sure to include all team members in checklist development. "It needs to make sense to the user, or they won't use it," she said. She also recommends tracking usage of the checklist and reporting on success and usage at MEC meetings, teammate meetings and medical staff meetings.
2. Develop tools and processes to support implementation. Ms. Bemis said the checklist will most likely need some tweaking before it's perfect for your facility. Try out the suggested checklist a few times, make changes, and then implement the final product. Once you decide to implement, model the usage of the checklist in a clear way.
You can develop tools to assist with follow through — SCA had developed toolkits, demonstration videos and training material to introduce teammates to the process of using the checklist.
3. Set clear expectations for individual accountability. Make sure you set clear expectations for teammate behavior. "Be clear about what top-level performance looks like," Ms. Bemis said. Make sure you go line item by line item and verify that you completed the items before you proceed with surgery.
4. Make the checklist part of your culture. Implementing a surgical checklist doesn't stop at handing out a piece of paper to staff members. You should regularly track usage of the checklist and talk about the effect on patients. When surgical errors or "near misses" occur, gather teammates together to talk about why they happened. Don't blame others, but call each other out on mistakes and omissions so you can avoid them in the future. And celebrate success and consistency — let your team members know that you appreciate their efforts.
***
It is incumbent upon surgery center leaders to develop a format of safe surgery checklists that will drive usage, Ms. Lansing said. "The other thing is that we need to carefully consider how to implement the checklist," she said. "Having a well-designed checklist doesn't mean that you'll have great pull-through on it." Consider culture as well as process; only a deeply ingrained safety culture will prevent serious surgical errors in the long run.
Access the audio recording of this webinar here.
Access the PDF version of the webinar here.
More Articles on Surgery Centers:
25 Statistics on Orthopedic Revenue & Changes in ASCs
6 Tips to Overcome Payor Concerns With Spine Surgery in ASCs
Opportunities & Trends for Opening ASCs Next Year: Q&A With Rebecca Harrell
History & justification for checklists
Ms. Lansing began the webinar with an overview of the history of the surgical checklist. "If you look at the literature, you'll see that the development of checklists from a professional point of view ties back to the aviation industry — and, most significantly, to the aviation industry during the 1930s and 40s," she said. During that time, airplanes were gaining more sophisticated technology in the cockpit, causing problems for pilots who had previously operated more simple machines. Though the technology was intended to improve safety, it was widely considered "too complicated" for a pilot to manage. The number of crashes during this time period attested to the high error rate.
In examining the behavior of pilots in these new planes, experts found that the pilots with the most flying experience were not always the ones with the best results. "We usually think that time and grade in a profession will go ahead and give us competence, and competence will drive … safety and good quality results," Ms. Lansing said. But the human brain is flawed, and even the best training does not prevent a pilot from forgetting a crucial task for take-off.
"They really began to consider: How do you deal with extreme complexity?" Ms. Lansing said. "How do you ensure you complete every step in the process, particularly when that process is done very frequently?" Interestingly, the more frequent and routine a process was, the more likely errors were to occur. As it turns out, when you've performed the same task a hundred times, you fall into a certain sense of complacency about double-checking your work.
To ensure that pilots didn't forget crucial steps, the aviation industry developed a series of checklists. At first, they were used as a memory aid: The pilot would go through and complete every activity, then refer to the checklist to make sure everything was done. It was eventually determined that a more effective approach was to go through the checklist step-by-step, reading each task out loud and attending to issues as they arose.
Why are checklists difficult to implement?
Atul Gawande is an American surgeon and journalist whose books include Better, Complications, and — most relevant to this subject — The Checklist Manifesto. He has advocated heavily for surgical checklists, arguing that the fallibility of human memory opens the door for serious, fatal errors when surgeons rely on their training alone.
Ms. Lansing said part of the difficulty in implementing checklists comes down to an attitude of individual autonomy in medicine. Surgeons, who have gone through years of training, often believe that good medicine is up to the talents of an individual physician — not the collective, systematic effort of a checklist. But studies have proven that checklists vastly reduce the incidence of surgical errors, so the question becomes not, "Should we implement a checklist?" but, "How do we do it?"
Ms. Lansing said team members should follow a "professional code of conduct," with three key characteristics:
• Selflessness. Surgeons and team members must put the needs of others above their own. This eliminates feelings of personal pride over using a checklist or double-checking with others.
• Strong skillset. Surgeons and team members must be well-trained in their field and able to execute tasks well.
• Trustworthiness. Surgeons and team members must be responsible for their personal behavior with others and present themselves as team players.
Dr. Gawande said airline pilots take this a step further. They add a fourth dimension: discipline. "They really feel it's part of being a professional to follow prudent procedures when working with others, because it's important that everyone involved in a process or procedure is operating in the same way," Ms. Lansing said. This idea is in stark contrast to the image of the maverick surgeon, but you can't argue with the results: Study after study says that it works.
"If you think about medicine, we have a tendency to place a great deal of value on autonomy," Ms. Lansing said. "We want to be autonomous and make individual assessments. [Dr. Gawande] challenges that that is actually… in direct opposition to discipline. Is it right and professional to put the needs of autonomy in front of the need for discipline?"
Medicare and accreditation requirements
Ms. Lansing turned the floor over to Ms. Bemis to discuss regulatory requirements for surgical checklists.
Last year, Medicare announced that ASCs would be required to start quality reporting in 2012. In addition to reporting the use of safe surgery checklists, surgery centers are required to perform quality metric reporting using G-codes, reporting whether patients have had transfers, falls, burns and other issues. While these metrics only apply to Medicare patients, the safe surgery checklist must be used on all surgical patients, and ASCs must report they used it for all payors.
For 2012, the initial year of data collection, ASCs may report "yes" if they used it during any part of the year. That means that if you haven't started yet, there's still time. In subsequent years, the ASC will have to use the checklist for the entire year to answer "yes."
ASC leaders will report their surgical checklist use on a secure area of the QualityNet website starting July 1, 2013 and ending Aug. 15, 2013. CMS does not provide a required form for the surgical checklist, so surgery centers can tweak the items to best fit their needs. "This helps to increase the likelihood of compliance," Ms. Bemis said.
CMS is not planning to include the use of the safe surgery checklist in its surveys, and no financial penalties will be incurred at this time. "But that could change — and it frequently does," Ms. Bemis said.
The Medicare requirements target safe surgery practices during three critical periods:
• Prior to anesthesia, including marking the site, identifying the patient, identifying allergies and airway issues, etc.
• Prior to incision, including the time-out process, the timely administration of antibiotics, etc.
• Prior to the patient leaving the OR, including debriefing, identifying concerns that arose in the operating room, etc.
"When we think about Conditions for Coverage requirements, they're really looking for the use of standardized procedures to avoid errors," Ms. Bemis said. "They want to see that you have a pre-procedure verification process to ensure all relevant documents and related information is available and correctly identified."
Accreditation requirements
Accreditation requirements vary slightly from CMS requirements, with slight differences between different accrediting bodies. The Joint Commission developed and publicized the use of a standardized checklist in 2003, later deciding to convert the checklist to universal protocol. The Joint Commission requires that ASCs:
• Conduct a pre-procedure verification process. This means making sure you have the correct procedure, patient and site and identifying that all items necessary for the procedure are present.
• Mark the procedure site. Use an unambiguous and consistent mark to identify the procedure site.
• Perform a time-out immediately prior to starting the procedure.
The Joint Commission has aligned its universal protocol with CMS requirements for a safe surgery checklist.
The requirements for AAAHC accreditation are slightly different again. The AAAHC requires that ASCs:
• Utilize a process involving the patient to identify and designate surgical procedure and surgical site
• Have the OR manager verify site, identity, procedure and that all equipment is available immediately prior to beginning the procedure
"There is a thread of similarities between organizations," Ms. Bemis said. She added that there are several sample checklists that ASCs can use or tweak as needed. One checklist comes from the World Health Organization and is divided into three components that reflect the original Medicare requirements. Another sample checklist, developed by AORN, has taken items from WHO and also considered items in regard to national patient safety goals. The AORN list is divided into four areas: pre-procedure check-in, sign-in, time-out and sign-out.
For any checklist, the key is simplicity. "An overly detailed checklist can became so unwieldy that it isn't used and actually gets in the way of getting things done," Ms. Bemis said.
Development and implementation: A checklist for using checklists
Ms. Lanisng showed the following list of ideas to implement a surgical checklist. This guideline for checklist format and structure was developed by Dr. Gawande and can be found in his book.
In order to implement a safe surgery checklist, she said four key components are crucial.
1. Engage actively with key stakeholders. Your key stakeholders in this situation are OR teammates and physicians, and everyone needs to work together to make a checklist effective. "If we have a lack of engagement in development of the checklist, that's the number one reason for poor follow-through," Ms. Bemis said.
Make sure to include all team members in checklist development. "It needs to make sense to the user, or they won't use it," she said. She also recommends tracking usage of the checklist and reporting on success and usage at MEC meetings, teammate meetings and medical staff meetings.
2. Develop tools and processes to support implementation. Ms. Bemis said the checklist will most likely need some tweaking before it's perfect for your facility. Try out the suggested checklist a few times, make changes, and then implement the final product. Once you decide to implement, model the usage of the checklist in a clear way.
You can develop tools to assist with follow through — SCA had developed toolkits, demonstration videos and training material to introduce teammates to the process of using the checklist.
3. Set clear expectations for individual accountability. Make sure you set clear expectations for teammate behavior. "Be clear about what top-level performance looks like," Ms. Bemis said. Make sure you go line item by line item and verify that you completed the items before you proceed with surgery.
4. Make the checklist part of your culture. Implementing a surgical checklist doesn't stop at handing out a piece of paper to staff members. You should regularly track usage of the checklist and talk about the effect on patients. When surgical errors or "near misses" occur, gather teammates together to talk about why they happened. Don't blame others, but call each other out on mistakes and omissions so you can avoid them in the future. And celebrate success and consistency — let your team members know that you appreciate their efforts.
***
It is incumbent upon surgery center leaders to develop a format of safe surgery checklists that will drive usage, Ms. Lansing said. "The other thing is that we need to carefully consider how to implement the checklist," she said. "Having a well-designed checklist doesn't mean that you'll have great pull-through on it." Consider culture as well as process; only a deeply ingrained safety culture will prevent serious surgical errors in the long run.
Access the audio recording of this webinar here.
Access the PDF version of the webinar here.
More Articles on Surgery Centers:
25 Statistics on Orthopedic Revenue & Changes in ASCs
6 Tips to Overcome Payor Concerns With Spine Surgery in ASCs
Opportunities & Trends for Opening ASCs Next Year: Q&A With Rebecca Harrell